Introduction
If you’ve noticed your teeth turning black, you’re not alone—and you’re not imagining things either. Black teeth can appear due to a range of medical issues, from something as simple as poor dental hygiene to more complex causes like pulp necrosis or enamel erosion. This article breaks down the scientific and clinical truths behind black teeth, how they develop, and most importantly, what you can do about them. Backed by insights from trusted medical sources like PubMed and the American Dental Association, we’ll explore causes, treatments, prevention strategies, and patient-friendly FAQs to help you protect your oral health.
Discover great ideas like daily oral care techniques backed by science.
Table of contents
PART 1: Understanding What Causes Black Teeth
– Dental Plaque and Tartar Accumulation
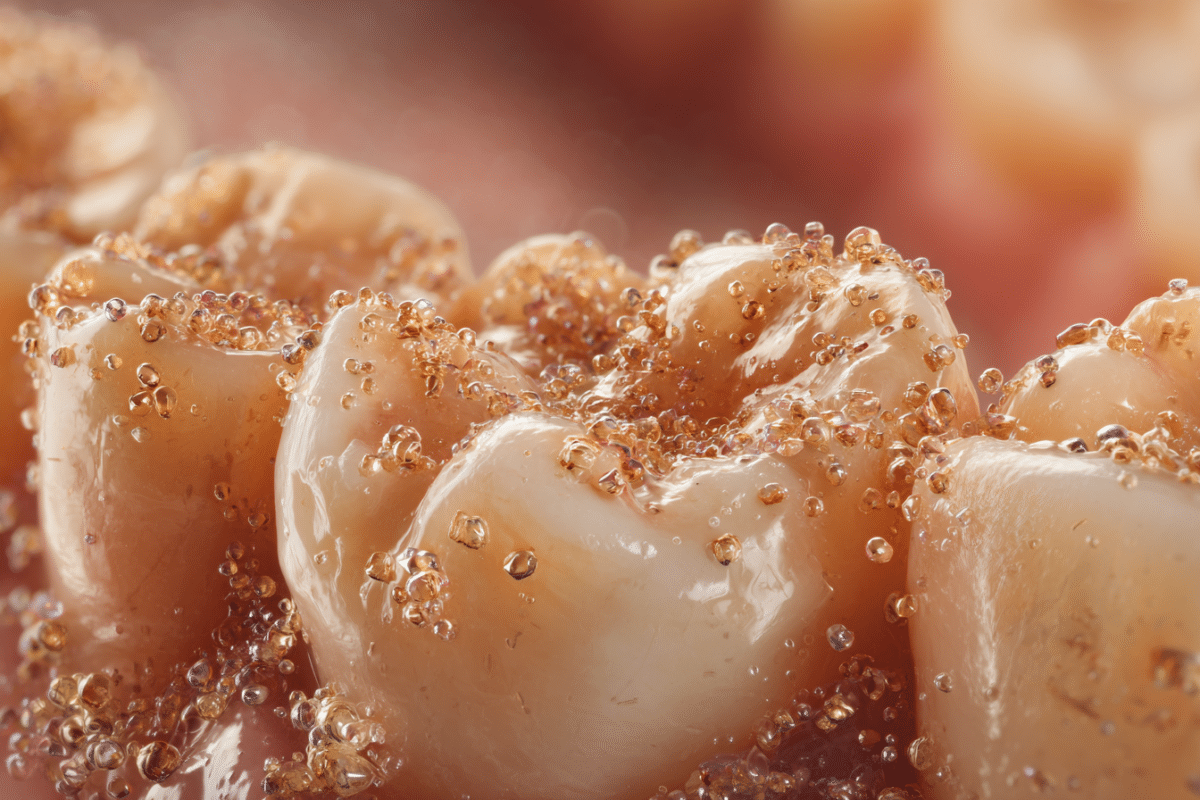
The most frequent cause of black teeth is the accumulation of dental plaque and tartar, especially when oral hygiene is neglected. Plaque is a sticky film composed of food particles and bacteria that naturally forms on your teeth. When not removed through regular brushing and flossing, it hardens into calculus, commonly known as tartar. Over time, tartar can absorb stains from beverages like coffee, tea, or red wine and appear dark brown or black.
The black coloring of tartar may also come from chromogenic bacteria, which produce pigments as they metabolize carbohydrates. These bacteria thrive in moist, low-oxygen environments such as the gum line or between teeth.
Clinical studies show that black tartar commonly forms on the lingual (tongue-facing) surfaces of lower front teeth, where saliva flow is reduced, and brushing is often less thorough. Dentists often remove this using ultrasonic scaling devices, which break apart the tartar without harming enamel.
According to PubMed, untreated tartar leads not only to cosmetic discoloration but also to gingival inflammation, periodontal disease, and even tooth mobility.
– Tooth Decay and Internal Deterioration
Another serious cause of black teeth is tooth decay. When bacteria penetrate through the enamel and reach the dentin or pulp of a tooth, they begin to destroy the structure internally. This process results in necrosis (death) of the tooth’s internal tissues.
As the soft tissue dies, it turns dark, and this color change may eventually be visible externally. This type of discoloration is typically localized to one tooth, often following trauma or a large untreated cavity. You might notice a dark gray or black shadow from inside the tooth, especially if the enamel is thin or damaged.
This internal darkening cannot be brushed away. The tooth often becomes sensitive or painful, signaling the need for a root canal, a procedure where the infected pulp is removed and replaced with a sterile filling.
In some cases, non-vital bleaching is used after a root canal to lighten the remaining discolored tooth structure. However, this is only possible under strict clinical guidelines.
Learn more about how pulp necrosis affects tooth coloration, especially in adult dentition and post-trauma patients.
PART 2: Medical Treatments for Black Teeth
– Professional Dental Cleaning and Scaling

If black teeth are caused by plaque or tartar accumulation, the first and most effective treatment is a professional dental cleaning. Dentists use specialized instruments, such as ultrasonic scalers, to break up and remove hardened tartar that has bonded to the enamel surface.
These tools vibrate at high speeds to dislodge tartar while flushing the area with a water spray. The result is a visibly cleaner tooth surface and healthier gums. A clinical study published in the Journal of Periodontology confirms that scaling and root planing significantly reduce inflammation and surface stains associated with black teeth.
After cleaning, a polishing step is often performed to smooth the enamel and reduce surface stain retention. In many cases, this non-invasive treatment can completely reverse the appearance of blackness caused by external staining or tartar.
Patients with severe tartar buildup may need multiple sessions, especially if black deposits have migrated below the gum line.
Check out scientific recommendations for scaling and its role in oral disease prevention.
– Restoration Options: Fillings, Crowns, and Root Canals
When black teeth result from tooth decay, internal necrosis, or trauma, simple cleaning is not enough. In these cases, restorative dental treatments are necessary to both repair the damage and restore aesthetics.
1. Fillings:
For black spots caused by early-stage decay, the decayed part of the tooth is removed and filled with a tooth-colored composite resin. This is a quick, effective treatment, and the result often looks like a brand-new tooth.
2. Crowns:
When a large portion of the tooth is black or decayed, especially on molars, a dental crown may be used. Crowns cover the entire visible part of the tooth, restoring both its appearance and function. Dentists usually recommend this when the structural integrity of the tooth is compromised.
3. Root Canal Therapy:
If the tooth has turned black due to pulp death or deep infection, a root canal is the gold standard treatment. The procedure involves removing the infected tissue, disinfecting the canal, and sealing it. The tooth may still appear discolored, so a crown or internal bleaching is often added for aesthetic improvement.
Root canal-treated teeth may require non-vital internal bleaching—a technique where a whitening agent is placed inside the tooth—to improve cosmetic outcomes. According to a study in the American Journal of Dentistry, this method is safe and effective when applied under professional supervision.
For more information on treatment decisions, don’t miss our clinical breakdown of restorative options for discolored teeth.
PART 3: Can Black Teeth Be Reversed or Healed?
– Tooth Discoloration vs. Tooth Death
Understanding the difference between tooth discoloration and tooth death is critical in deciding whether black teeth can be reversed. Discoloration, especially from external staining or tartar, is usually reversible through dental cleaning or whitening. In contrast, when a tooth turns black from the inside due to necrosis or pulp infection, the situation is more complex.
Dead teeth cannot regenerate. The internal tissues, once necrotic, don’t “heal” like a skin wound. When a tooth dies, the only solution is root canal therapy or extraction. So while black teeth stains on the enamel can often be removed, actual tooth blackening from death or deep decay requires dental intervention, not natural healing.
Clinical literature published in Operative Dentistry shows that dentists must first determine whether the discoloration is intrinsic (from within) or extrinsic (on the surface) to choose the appropriate treatment method. A tooth vitality test using cold stimuli or electric testing helps determine if the pulp is alive or necrotic.
This distinction is vital to know whether the black tooth can be saved.
– Whitening Options for Superficial Black Stains
When black teeth are caused by surface stains from tobacco, coffee, wine, or plaque, whitening treatments can help restore their appearance. These stains typically reside in the outer enamel layer and can be lifted using hydrogen peroxide-based whitening agents.
In-office whitening is stronger and produces quicker results. Dentists use a concentrated whitening gel activated by light to break down the dark pigment molecules. The American Dental Association notes that this treatment is safe and effective when used under professional supervision.
At-home whitening kits may include trays, gels, or whitening strips. However, overuse or improper application can lead to sensitivity or enamel erosion, particularly if the black discoloration masks a cavity.
In some cases, microabrasion or enamel polishing can remove very shallow black stains. This is often used for black spots caused by early plaque accumulation or iron-rich foods.
Discover great ideas like professional bleaching systems and their clinical success rates.
PART 4: Preventing Black Teeth Through Proven Medical Practices
– Daily Oral Hygiene That Works

Preventing black teeth starts with consistent oral hygiene. The American Dental Association recommends brushing twice a day with a fluoride toothpaste and flossing daily. These steps help remove plaque before it hardens into tartar and turns black.
Using an antibacterial mouth rinse can reduce the population of chromogenic bacteria responsible for black staining. Fluoride rinses also strengthen enamel, making it more resistant to acid attacks from plaque biofilm.
Regular dental check-ups, ideally every six months, allow for early detection and removal of any dark deposits before they worsen. Professional cleanings not only brighten teeth but also prevent periodontal disease, a key risk factor in tooth discoloration and tooth loss.
According to the Journal of Clinical Periodontology, patients who maintain strict oral hygiene routines are less likely to develop black teeth or advanced decay. Additionally, using electric toothbrushes with pressure sensors ensures thorough but gentle cleaning—especially in hard-to-reach back molars.
– Diet, Smoking, and Medical Risk Factors
Beyond hygiene, your lifestyle and systemic health play a major role in preventing black teeth. Foods and drinks high in chromogens and tannins (like tea, red wine, berries, and soy sauce) contribute to dark stains. Limiting these, or rinsing with water after consumption, can help.
Tobacco, in any form, is a major contributor to black teeth. It not only stains enamel but also encourages tartar buildup and gum disease. According to CDC data, smokers are up to 3 times more likely to develop severe periodontal conditions that lead to black teeth.
Certain medical conditions like diabetes, dry mouth (xerostomia), and GERD also increase risk. Saliva plays a crucial role in neutralizing acids and cleansing the mouth. When saliva production is low—whether due to illness or medication—bacteria thrive, and staining accelerates.
Patients with iron supplements, especially in liquid form, or medications like tetracycline, may develop black or grayish stains over time. These should be discussed with your healthcare provider to adjust dosing or formulations if necessary.
Don’t miss our guide on systemic factors affecting oral health, especially in adult and elderly patients.
Advanced Insights and FAQs on Black Teeth
Teeth can go black for several reasons, ranging from harmless surface staining to severe internal damage. The most common cause is tartar buildup. When plaque isn’t removed, it hardens into tartar, which can absorb pigments from food, beverages, or tobacco, turning black over time.
Another major cause is tooth decay, which starts as a small cavity but, if untreated, penetrates deep into the tooth, eventually causing the pulp (nerve tissue) to die. The dead tissue darkens and stains the tooth from the inside. Trauma can also cause a tooth to die and blacken.
Certain medications (like liquid iron or tetracycline), medical conditions (such as GERD or diabetes), and smoking are additional contributors. In rare cases, genetic disorders affecting enamel or dentin development may also cause dark tooth discoloration.
Learn more about oral pathology and causes of tooth discoloration on PubMed.
Yes—but the treatment depends entirely on the cause. If the blackening is from external sources like tartar, coffee, or smoking, then a professional cleaning and polish can often restore the tooth’s natural color.
If the black areas are from decay, they need to be removed and replaced with fillings, onlays, or crowns depending on the extent of damage. In case the tooth has died and turned black from the inside, root canal therapy may be necessary to clean out infected tissue.
For discoloration that remains after medical treatment, cosmetic solutions such as internal bleaching or veneers may be recommended. Only a dentist can determine the right course of action.
No, a black tooth that has died cannot heal on its own. Teeth do not regenerate in the way bones or skin do. If the cause is a dead nerve or internal infection, healing requires intervention, typically with a root canal to remove the infection and save the structure of the tooth.
However, a black tooth due to external staining or tartar can be treated and improved. Once the deposits are removed and the surface cleaned, the tooth may return to a healthy appearance.
So while not all black teeth can be “healed” in the traditional sense, many can be restored medically or cosmetically with professional care.
It depends. You can undo some types of teeth blackening, especially those caused by surface stains from coffee, wine, smoking, or tartar. These can be reversed using scaling, polishing, and sometimes whitening.
However, intrinsic blackening, like that caused by tooth death or decay, is not reversible in a natural sense. Instead, it requires dental intervention, such as a root canal, filling, or crown. In these cases, the blackening can be “undone” in the sense that the appearance and function of the tooth can be restored—but not without treatment.
Avoid DIY remedies, as they may mask symptoms without treating the root cause and could worsen damage.
Temporarily dyeing your teeth black is sometimes done for theatrical or costume purposes. Safe ways to do this include using non-toxic food coloring or products specifically designed for dental use, such as tooth wax paints or mouth-safe dyes used in acting.
Never use ink, permanent markers, or activated charcoal for long durations, as they can damage enamel and irritate the gums. Always read the label and ensure the product is FDA-approved or intended for oral use.
And remember—this should always be a short-term, cosmetic-only measure.
Black tartar, also called calculus, cannot be removed by brushing alone once it has hardened. The only safe and effective way is through professional dental cleaning.
During the cleaning, a dental hygienist uses manual scalers or ultrasonic tools to break apart the calcified plaque without harming the enamel. The procedure is painless and essential to prevent gum disease and further tooth damage.
Home tools and scraping methods are not recommended and may cause injury or increase the risk of infection. Schedule a cleaning every 6 months to keep tartar at bay.
In adults, black teeth typically develop due to years of accumulated factors such as:
Poor oral hygiene
Long-term tobacco use
Excessive coffee, tea, or wine intake
Lack of professional dental cleanings
Gum disease or periodontitis
Tooth trauma or decay
Systemic illnesses (e.g., diabetes)
Side effects from medications like iron supplements or tetracycline
Older adults are more likely to develop receding gums, which expose root surfaces where tartar and stains accumulate faster. This is why consistent dental care and early treatment are key to prevention.
Black spots can mean different things: they may be superficial stains, early cavities, or remnants of tartar. The treatment depends on the diagnosis:
Surface stains: Polishing or whitening
Early decay: Dental filling or fluoride varnish
Old fillings or sealants: May need replacement if deteriorating
Your dentist may use digital imaging or bitewing X-rays to determine the depth of the spot and decide whether it’s purely cosmetic or a sign of deeper decay.
To remove black stains, first get a professional evaluation. If stains are extrinsic (on the enamel), dentists may use:
Scaling and polishing
Air abrasion
In-office whitening
Whitening trays for at-home use
If the stains are intrinsic, involving the dentin, treatments may include internal bleaching, veneers, or crowns.
Avoid DIY mixtures of baking soda and lemon, as they are abrasive and acidic—this will damage your enamel over time.
Looking for inspiration? Try clinically proven whitening protocols and research.
